
WHY Patient Right to Autonomy Act?
Every life is uniquely valuable, and every decision made regarding your life should be respected and protected. This is the reason why PSDA came into being.
Patient Right to Autonomy Act is the first patient-centered act. In the act clearly states that every patient has the right to know, to choose and to decide personal medical decisions. For those who have made their Advance Directive (AD) decisions and later fall into a coma or become too ill to make decisions, their autonomous wills will be protected by the law and carried out. When later your health condition deteriorates and meets the five clinical statuses (e.g., end of life stage, persistent vegetative state, and etc.), you can decide if you wish to prolong your life through medical interference or choose palliative care to ensure a quality death .
Through this expression of patients’ medical choice, autonomy and dignity are being respected while the right of a good death is being protected. Patients, family members and the medical team can all learn to understand the patients' true desires via the Advance Care Planning (ACP). This will help achieve the harmony between doctor-patient relationships, and also alleviate the grief and loss. By returning the right of decision-making back to the patients, this also eases the guilt for the bereaved and helps them to realize they are helping their loved ones by supporting their decisions.
In addition, this Act provides medical professionals a clear legal basis to follow when the five clinical status mentioned in the Act are encountered.
A Comparison chart between Patient Right to Autonomy Act and the current Hospice Palliative Care Act (HPCA)
Hospice Palliative Care Act only protects the right of medical decisions of the terminally ill patients; however, this Act has added four new targets. Additionally, when signing the current Letter of Intent, HPCA requires only the patient and two witnesses; whereas the Advance Directive mentioned in this Act will require an Advance Care Planning consultation process provided by the medical institute. Both will be registered in the National Health Insurance system.
|
Aspects |
Hospice Palliative Care Act |
Patient Right to Autonomy Act |
|
Concept |
1. Protect patient's right of a good death |
1. Protect one's dignity, autonomy and right to a good death. People with a sane and sound mind can make their own decisions; |
|
Criteria |
Terminally ill only (advanced cancer and eight non-cancer diseases) |
Five types of clinical status: |
|
Scope |
1. Resuscitation |
1. All medical treatments that may possibly prolong patients’ lives, including: resuscitation, life-sustaining devices, blood, antibiotics, and etc. |
WHY do I need it?
The current Medical Care Act states: “Medical care institutions shall explain … to the patient or his/her legal agent, spouse, kin, or interested party, and must obtain his/her consent….” This seemingly appropriate statement actually hinders the medical team from explaining the patient's condition to himself/herself, and often does not reveal the whole truth. Both having a patient who does not know his own health condition and family members who are not able to have a meaningful conversation with the patients are not only a waste of valuable and short remaining time, but also a failure to provide for the patient to fulfill his last wishes. Although this Medical Care Act arose out of the love to patients, it has often ended up wasting precious time and causing regrets to both the living and the dead.
Patient Right to Autonomy Act, on the other hand, has a clear patient-centered position to protect patients' right to know by stating that patients have the right to know the diagnosis, medical options, and the consequences and risks that follow. Only when patients do not strongly express objection can the medical team inform the patients' personal medical information with other related parties.
HOW does it work?
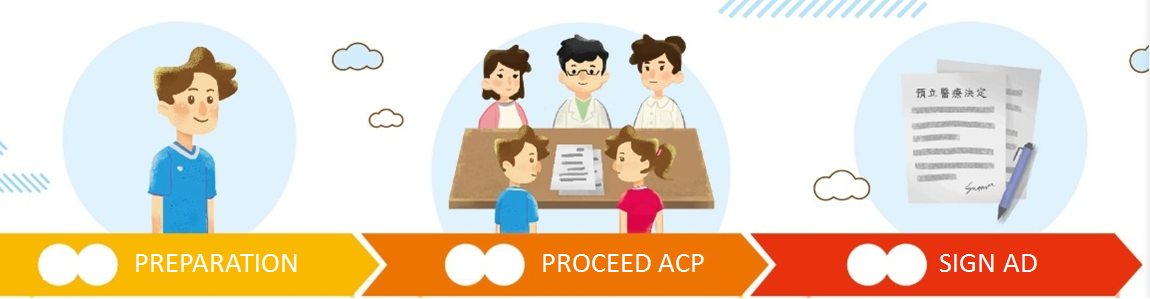
Anyone over 20 years old with full capacity can create an Advance Directive with the following steps:
- Make a reservation for ACP consultation in assigned hospitals;
- Make sure to show up in the consultation meeting and bring your medical attorney with you (if any) and open up your mind for the coming candid discussion;
- Stamped by the assigned hospitals and notarized by a notary public or signed and witnessed by at least two witnesses;
- Registered in the National Health Insurance.
WHERE can I receive ACP consultation?
For eligible medical institutes that fit to provide Advance Care Planning consultation, please see the updated list announced by MOHW.
https://hpcod.mohw.gov.tw/HospWeb/RWD/PageType/acp/HospitalMap.aspx
病人自主權利法20問PDF(超連結)

