The minimum need for a terminally-ill patient is to be comfortable, and to achieve this, the first step is to reduce the patient’s pain to its minimum. In a research done in 1999, I came to the conclusion about the ten most important criteria to assist in a patient’s dying well, and the top priority is reducing pain and discomfort. If the pain cannot be relieved, the patient often feels melancholy and helplessness, and thus remains in a constant state of depression, sadness and loneliness. Having experienced pain already, the patient becomes anxious and fears any recurring pains. This anxiety lowers the patient’s tolerance for pain and weakens the will to live.
In the past, it is said that patients so desperately ask for anesthesia that they even beg physicians and nurses. At times, they may even wander from hospital to hospital in their desperate search to obtain it. This is not fiction, but true, tragic stories that happen everywhere.
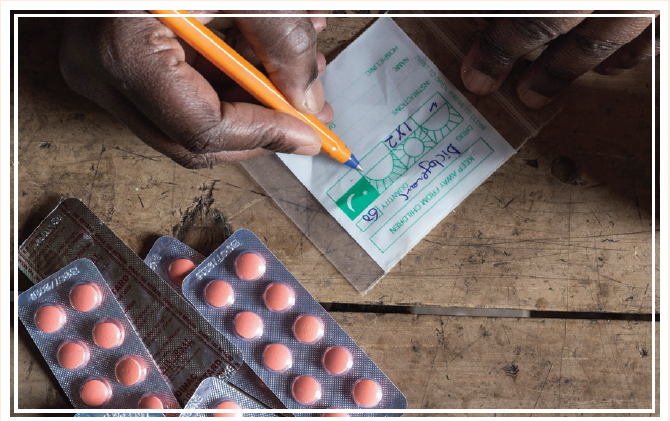
Today, the medical circles have made enormous improvements with effective pain management, and also corrected many misconceptions. World Health Organization published the 3B and 3R principles. 3B refers to the WHO Ladder which includes By the Ladder, By the Mouth, and By the Clock. By the Ladder means to provide medicine in three steps, from non-opioid, to mild-opioid, and finally to strong-opioid. With each step is the combined use of an adjuvant. In addition to eradicating the misconception that patients should endure as much pain as possible, patients should take medicine as the last resort so as to avoid addiction. If patients with chronic diseases need to endure pain until it is unbearable, by the time the medicine intervenes, it often requires heavier doses, and the constant pain will also wear out the patients' tolerance and faith. They might end up relying on pain killer medicine even more.
As for 3R, it means Right Drug, Right Dose, and Right Interval. The modern pain management for chronic diseases has changed from previously providing medicine when patient feels pain to nowadays taking medicine regularly. The medicine will be given through less intrusive ways, starting with oral dosage, then to subcutaneous injection,
then to skin patches, and finally to anal suppository. The specific use of any drug and its dosage will also need to be evaluated based on the individual patient’s condition.
When it comes to relieving pain, medicine is not always the only option. There are some supplementary treatments that can also effectively ease and relieve pain. Some examples include relaxation techniques, acupuncture, Transcutaneous Electronic Nerve Stimulation(TENS), shiatsu, physical therapy, rehabilitation, music and art therapy, even humor, aroma, spiritual and religious care can all offer the same merit that has been proven scientifically and with documented support.
I always ask my audience why it is terrifying to have an incurable disease. Are we afraid of dying, pain, losing our dignity and quality of life? Or are we afraid that we might be a burden to our loved ones? Actually, most people are afraid of pain more than death, and as such, enduring unnecessary pain is an inhumane and meaningless suffering to the terminally-ill patients. Only when we assist patients to manage their pain effectively, can we help them to reclaim the quality of their lives.
Even though pain management has greatly improved, the general public is more informed of palliative care knowledge, and honor has been bestowed by the Lien Foundation’s Quality of Death, problems remain. The current Taiwanese hospitals that provide palliative care are now serving around 170,000 end of lives per year, but with rather scarce human resources as well as lack of training and facilities. Additional problems include the significant reduction of professional training hours, low nurse-to-patient ratios even when health coverage has been increased, and the decline of overall palliative care standards.
If we lower the standards of palliative care in order to provide palliative care to more regions and patients, I would ask this question: "Is lower standard palliative care what patients expect to receive?" The answer is based on the fact that high-quality palliative care hospitals have no beds to spare while lesser-quality palliative care hospitals remain at below 30% in ward occupancy. It is clear what patients want as they have made their decisions toward higher quality palliative care, and we must respond by providing high-quality palliative care.