Who could have predicted the COVID-19 pandemic was coming? The medical staffs on the front line against the virus are shouldering the heavy responsibility of pandemic prevention, taking care of the infected patients with their professionalism and sense of mission, and carefully watching various life situations at the clinic during the pandemic emergencies. This article invites two professional nurses to share their personal experiences and heart-warming life stories that occurred among the medical staff, patients, and their families.
Facing Life and Death with Bravery and Gentleness
With extensive experience in hospice and palliative care, Taipei Tzu Chi Hospital’s Chief Nursing Officer, H.N. Mei-Hui Chen participated in the fight against SARS in 2003. Eighteen years later when the COVID-19 pandemic broke out, she became a member of the wards that were dedicated to COVID-19 patients. She believes, "Due to the previous training for SARS, the expertise and confidence in medical care and pandemic prevention have improved a lot.” Nonetheless, the COVID-19 virus is especially tricky as the challenges have been overwhelming, and those heartfelt stories that start with genuine love and care have mostly been told in the isolation wards.
Turning Lifeless Dolls into Life-giving Companions
"Once confirmed to be infected, one has to stay in an isolation ward for at least 10 days. Whether he or she can survive this period becomes the patient's greatest fear," acknowledges H.N. Mei-Hui Chen. She once listened to a confirmed COVID-19 patient express his fears: "It felt like being in jail, and every day I was worried about not being able to survive. When I was short of breath, I was scared, feeling like I was dying. I didn't even dare to close my eyes at night because I was so afraid that if I fall asleep, I would never wake up again."
On top of that, in a closed and isolated environment, it is easy to feel panic, fear, and restraint. H.N. Mei-Hui Chen once met an elderly female patient, who had been diagnosed with dementia. Faced with an unfamiliar space in the ward, she was agitated and restless. Not only did she nag about the same problems repeatedly, she would also knock on the door incessantly, causing quite a commotion: Boom, Boom, Boom! Additionally, she pulled on the locked doorknob, trying to rush out of the room if the door should open. Despite many attempts to calm her down, nothing worked.
So the team asked the patient’s daughter and learned that as long as she has some company--even if together in total silence- -her mother could be comforted. Unfortunately, at that time almost all the hospital staff was devoted to saving lives, so how could there be any extra staff member to be with her? Then it clicked… the hospital staff found a life-sized inflatable doll. They dressed it up with personal protective clothing, a mask, and gloves; and carefully drew the facial features before placing it next to the hospital bed. Seeing a person beside her, the old lady indeed calmed down, cooperated with receiving the medications and treatments, and left the quarantine unscathed.

"Actually, the elderly patient knew outright that the doll was not real person from the medical staff," says H.N. Mei-Hui Chen. One time the doll had deflated, so our staff member picked up an oxygen cylinder to inflate it back up. At that time, the elderly patient even offered to help! When someone asked her, "Grandma [honorific title for an elderly woman] are you happy that we invited a nurse to stay with you?", she grinned with gratitude and responded, "Yes!"
Devoted to Give Patients Maximum Care
During the severe pandemic, many confirmed patients were sent to the hospital alone, with only medical staff there with them to spend the darkest moments of their lives. Therefore, in addition to empathizing with patients’ emotions and needs, the medical staff must be keenly sensitive to cope with emergencies.
For example, a vagrant, who had been wandering around for a long time, continued to sleep on the floor even after being admitted to the ward. The nursing staff coped with his living habits and kneeled on the ground to take his blood pressure, give him shots, and perform other treatments. When his health condition suddenly worsened, at the risk of hurting their backs, the nursing staff carried him onto the bed together, assisted him in eating, drinking, turning over, and changing diapers. They took good care of the patient and took photographs to periodically record his conditions.
After the patient passed away, H.N. Mei-Hui Chen washed and prepared his body for burial. As she rummaged through his baggage and found nothing inside, she asked the social workers for a complete set of clothes and whispered in the patient’s ear, "Sir, you can rest in peace now." Later, the police contacted his brother, who had been out of touch with the patient for many years. He was moved to tears when he saw photos of his dying brother, which eased some of the regret that he could not be with his brother in the last moments of his life.
On another occasion, H.N. Mei-Hui Chen cared for a drug addict. He smoked three packs of cigarettes a day, and when admitted to a non-smoking isolation ward, he fell into an unbearable, emotional turmoil. He once pulled out the door lock with his bare hands and sneaked out; he even attacked the parole staff, which caused a great disturbance. In his situation, the team could not administer sedatives or tie his hands and feet to the bed as they otherwise did to regular patients for fear that it would affect the lung function of the infected person. Doing so could even induce hypostatic pneumonia, which would be really hard to deal with.
It wasn't until H.N. Mei-Hui Chen communicated with the patient about the follow-up care policy that the situation began to improve. Putting a cigarette on the tip of the patient’s nose for him to smell, with a smoking cessation inhaler in his mouth, she managed to help him eliminate his tobacco addiction. After the patient quit smoking, he turned to eating to satisfy his desire with food, and thus, H.N. Chen provided a large amount of meals and snacks to relieve the patient’s anxiety and tension. He soon recovered and was discharged from the hospital because he cooperated in the treatment and even followed the suggestion of doing simple exercises in the ward.
Helping Patients with the Well-being of Their Body, Mind, and Spirit
Ms. Dai-Yuan Jiang, a nurse at Taipei MacKay Hospital, who had served in the intensive care unit for nine years and later transferred to the hospice ward, came to assist at the COVID-19 Intensive Care Unit in late May this year. Describing the scene, Ms. Jiang said, "It is like going to the battlefield." Each day from morning to evening with personal protective equipment on, unable to drink water or go to the toilet on time, the team faced the big challenge to relieve the isolated patients of their emotional and psychological pressure.
Prior to the pandemic, encouragement from family members and medical staff is usually sufficient to help patients ease their anxieties. However, with the onset of the pandemic, the hospital no longer allows visits, and close contact has become a luxury. Ms. Dai-Yuan Jiang can only seize what limited time is available in the ward chatting with the patients while working to guide them through depression, asking questions such as: “What do you want to do most after your recovery?” She hopes they will feel more hopeful and cheer up enough to endure the difficulties. Observing the dynamics through a monitor, if she finds the patients’ condition is not so good, she will turn on the intercom to comfort them, letting them know that they are not alone, and that the nursing staff outside are silently caring for him.
She also allows patients to communicate with relatives and friends through telephone and video conferencing to reduce anxiety; this way, she is also able to learn more about the patients’ preferences. For example, there was a patient who had a strong religious faith. After Ms. Dai-Yuan Jiang discussed with his family, they decided to put poems and his favorite pop songs in MP3s and recorded greetings and heart-warming words from the whole family. The patients played them when they could not meet each other, and the feeling of being loved and cared for helped the patient navigate through his negative emotions.
Ms. Jiang also lamented that the COVID-19 virus is very difficult to deal with. In particular, invisible hypoxia is the most difficult to predict. It is often the case that one appears normal at first, but then suddenly become very ill. However, the patient himself is not aware of any discomfort and quickly faces the critical moment between life and death. For example, an elderly woman was intubated due to a rapid drop in blood oxygen concentration. The medical staff judged that with their best effort, there was a chance to restore her life. However, she mistakenly believed that the intubation would likely kill her and thus refused. Later, the nursing staff urgently contacted her family who could not be present, and after the communication, the elderly woman was finally willing to be intubated so she could breathe with a ventilator. After spending nearly two weeks in the intensive care unit, her condition gradually stabilized.
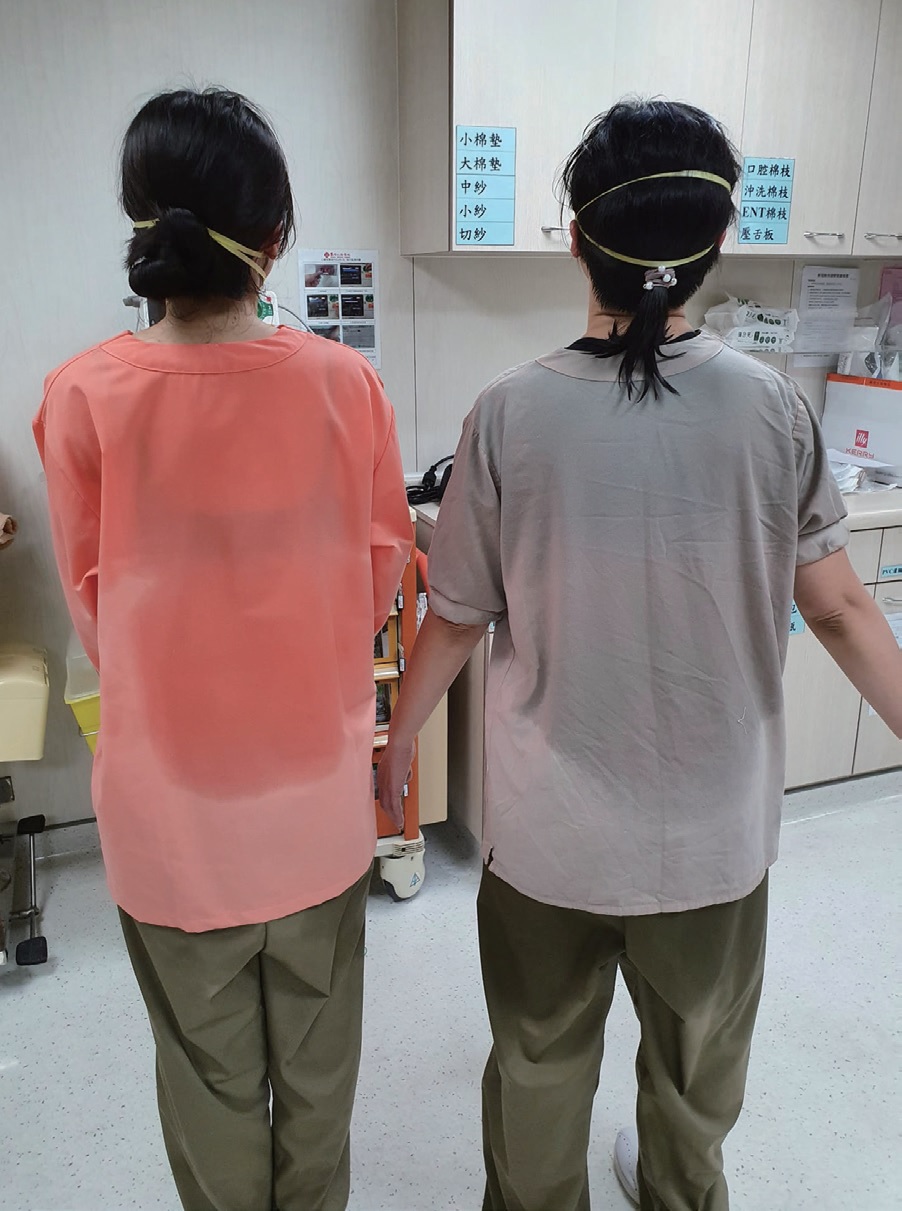
Ms. Dai-Yuan Jiang also shared how this elderly female patient loved to look beautiful in appearance; she even dyed her long hair a bright purple color! The moment she was detached from the ventilator and climbed out of bed, she insisted to wash her hair. So Ms. Jiang and another colleague gathered all the bathing items, helped the patient to the bathroom, and gave her a good bath. They combed and loosened her knotted hair, which made the patient shout out loudly and happily, "My illness and mood are halfway to recovery!" She then immediately video-conferenced with her family. Watching her show off her long and shining purple hair with joy, the two nurses covered and sweating in their personal protective clothing could not help but laugh along.
Sudden Farewells, but Love Is Always Present

When illness comes quickly, it can cause many regrets if one misses the opportunity to say goodbye. Such was the case for the elderly man, who did not recover after intubation. When his children arrived, their eyes filled with tears, and they begged, "Can I go inside and hug him?" Though not possible, the team compromised to allow the family members turn on the monitor and the intercom to express their love for their father in this way, with only the glass door in between. "When the handset was picked up, everyone in the room couldn't help crying out loudly." It is quite heartbreaking for one to not accompany family members in person at the end of the life journey; it can be really difficult to accept.
What Ms. Dai-Yuan Jiang had not expected was that a similar situation would happen to her own family. Her 90-year-old aunt, a distant relative, was confirmed to be infected with COVID-19. When she was sent to the hospital, she was suffering severely, and her outlook was not too optimistic. Furthermore, she did not wish to be intubated. Her children abroad could not come back in time, so they could only thank their mother, apologize for not being with her physically, and express their love through video-conferencing. Watching her beloved aunt nodding and shaking her head strenuously in the conversation, and her children crying their last farewells, Ms. Jiang, shifted her role from being a medical staff to a family member; she was deeply moved. "After all, no one can accept the death of a loved one so suddenly."
"There’s still a lot to learn," says Ms. Jiang as she reflected on her month-long work at the intensive care unit. She believes that it is a valuable experience for nurses from different departments to have this opportunity for exchange and to learn together. For example, she had taken care of an elderly woman who agreed not to receive first aid. Although her condition could not be reversed, she still gently cleansed, applied lotion to, and massaged her, so that the patient could leave comfortably and peacefully. Seeing it, other nursing partners exclaimed, "So it can be done this way!" and they applied this loving care to other patients of their own.
With the pandemic lingering around, the spirit of hospice and palliative care is even more critical and precious than ever before. In addition to soothing the body, mind, and soul of patients, the grief of family members and medical staff also urgently needs to be attended to and comforted. It is believed that after the battle with COVID-19, our society will gradually grow and mature in the future because we have inspired one another with our life stories, which will continue to shine with genuine love and care for more patients to come.
