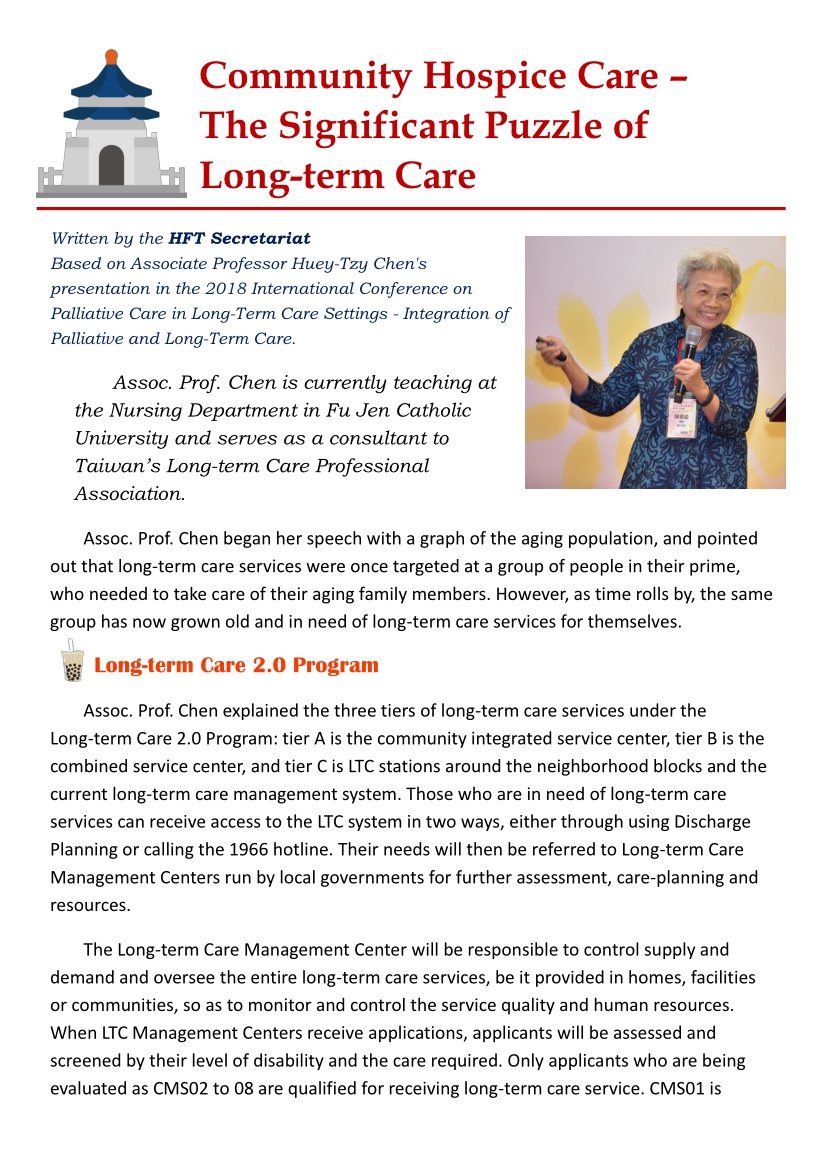
Assoc. Prof. Chen is currently teaching at the Nursing Department in Fu Jen Catholic University and serves as a consultant to Taiwan's Long-term Care Professional Association.
Assoc. Prof. Chen began her speech with a graph of the aging population, and pointed out that long-term care services were once targeted at a group of people in their prime, who needed to take care of their aging family members. However, as time rolls by, the same group has now grown old and in need of long-term care services for themselves.
Long-term Care 2.0 Program
Assoc. Prof. Chen explained the three tiers of long-term care services under the Long-term Care 2.0 Program: tier A is the community integrated service center, tier B is the combined service center, and tier C is LTC stations around the neighborhood blocks and the current long-term care management system. Those who are in need of long-term care services can receive access to the LTC system in two ways, either through using Discharge Planning or calling the 1966 hotline. Their needs will then be referred to Long-term Care Management Centers run by local governments for further assessment, care-planning and resources.
The Long-term Care Management Center will be responsible to control supply and demand and oversee the entire long-term care services, be it provided in homes, facilities or communities, so as to monitor and control the service quality and human resources. When LTC Management Centers receive applications, applicants will be assessed and screened by their level of disability and the care required. Only applicants who are being evaluated as CMS02 to 08 are qualified for receiving long-term care service. CMS01 is defined as “frail” and will be referred to rehabilitation services. Furthermore, a questionnaire with 34 questions will be used to better identify what kind of care is needed.
According to the current Long-term Care 2.0 Program, the cost of service will be split between the government and the beneficiaries. The percentage of cost that needs to be paid by the beneficiaries will depend on their household income level. In order to better take care of caregivers and encourage more young people to participate in this industry, the payment for caregivers has been revised to the current package deal from the original package deal of being paid per visit.
The revised package deal payment allows the caregivers to focus more on professional care; for instance, swallowing and feeding care, rehabilitation and nutrition care, rather than the usual daily routine care.
Hospice and Palliative Care
Hospice and Palliative Care service has been provided in Taiwan since 1990 and is covered by National Health Insurance. Assoc. Prof. Chen presented a demand forecast from a Taipei City Hospital research published by Dr. Chao-Ming Huang (2015), which shows that the demand for palliative care service for non-cancer patients will rise significantly in the years to come. According to this statistics, the coverage rate for cancer patients to receive palliative care is now 55-56% in 2016; however, it is relatively low for non-cancer patients. If palliative care can be provided in the long-term care setting, the beneficiaries will greatly expand.
The original palliative care system that focuses on the hospital setting will be unable to meet the demand, and thus it is vital to expand palliative care services to the community setting and institutional setting in order to include more elderly. The system flow for palliative care in community setting is now constructed and steadily functioning.
Looking Ahead: Connecting Long-term Care with Palliative Care
Assoc. Prof. Chen also shared two case studies of long-term care patients, who received palliative care at home at their own expenses.
These cases indicate that demand for palliative care existed among long-term care patients, but they did not have access to palliative care services. In considering the integration of the two current systems, long-term care service and palliative care, Assoc. Prof. Chen pointed out the compatibility issue of each assessment tool as related to CMS and palliative needs assessment. She also proposed ways to integrate the financial aspects of a combined policy within the NHI coverage and payment. As the Patient Autonomy Act will be enforced in 2019, her speech is timely to reconsider the distribution of resources and ease of access to those in need.