Taiwan continues to have a high rate of nasogastric tube usage. Among hospitalized patients over the age of 65, the rate is 18%, and in long-term care facilities, it rises dramatically to 94.05%—the highest in the world. Nasogastric tubes not only cause physical discomfort but also rob patients of the pleasure of eating, impacting their dignity and overall quality of life.
In 2017, renowned Taiwanese author Chiung Yao refused the use of a nasogastric tube for her husband, Hsin-Tao Ping, who had dementia. Her decision led to a highly publicized conflict with her three stepchildren, known in the media as the Intubation War. The case ignited nationwide discussions on end-of-life dignity and medical choices, with much of the debate centered around nasogastric tubes: When are they necessary? Are they the only option? And can they be removed once inserted?
When patients experience swallowing difficulties due to conditions like stroke, dementia, or aging, oral intake can lead to choking and aspiration pneumonia. To reduce this risk, the standard medical solution has been to insert a nasogastric tube, allowing food and medication to bypass the throat and go directly into the stomach. This ensures nutrition and sustains life, but often at the cost of comfort and normalcy.
A nasogastric tube is a long, flexible plastic tube inserted through the nostril, down the throat and esophagus, and into the stomach. A portion of the tube remains visibly attached to the face, resembling an elephant trunk. Aside from its awkward appearance, the presence of this foreign object often causes significant irritation and discomfort for patients.
Taipei City Hospital
Pioneering an Interdisciplinary Dysphagia Team
Swallowing disorders are especially common among patients with stroke, dementia, or advanced age. "But most hospitals don't have a specific Swallowing Department, so patients often don't know which specialist to consult," says Dr. Ya-Ling Li, Deputy Director at the Songde Branch of Taipei City Hospital and leader of the Dysphagia Team.
Taiwan's healthcare system is highly specialized, and the swallowing mechanism involves expertise from multiple disciplines. Previously, swallowing issues were addressed separately: stroke-related cases were diagnosed by neurologists and referred to speech therapists, while age-related difficulties often went unnoticed, with families attributing them to poor appetite and seeking help from gastroenterologists instead.
The standard medical approach to swallowing difficulties has traditionally been the placement of a nasogastric tube. However, with evolving medical perspectives, global healthcare policies have increasingly focused on training patients to regain swallowing function and reducing the number of patients reliant on tube feeding. "We realized that a multidisciplinary team approach was necessary to provide patients with more comprehensive treatment while gradually reducing the need for nasogastric tubes," says Dr. Li.
In 2018, under the leadership of former Taipei City Hospital President Dr. Sheng-Chien Huang, Taipei City Hospital integrated key departments related to chewing and swallowing function—such as dentistry, rehabilitation, otolaryngology (ENT), and neurology—along with healthcare professionals including dietitians, speech therapists, and social workers. This led to the creation of Taiwan's first Multidisciplinary Swallowing Team of Taipei City Hospital, comprising nearly 100 professionals from various disciplines across six hospital branches. Dr. Ya-Ling Li, a dental specialist, coordinates the team's efforts across departments.
Aging Can’t Be Reversed, But Swallowing Can Be Rehabilitated
When addressing dysphagia, Dr. Jun-Jie Wu, Director of the Rehabilitation Department at Taipei City Hospital Zhongxing Branch and a member of the Dysphagia Team, categorizes treatment into two approaches: prevention and improvement.
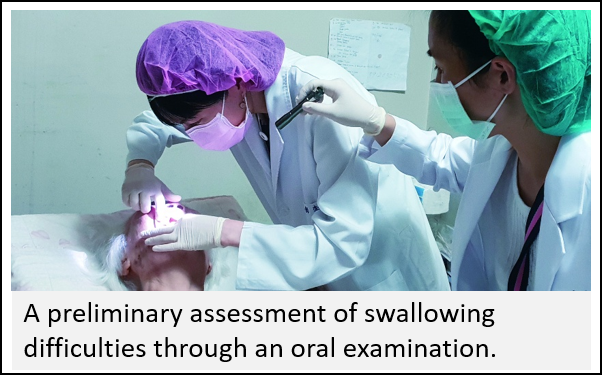 For younger individuals or those with early symptoms, performing swallowing and oral exercises can help maintain and improve swallowing function. The team conducts comprehensive assessments based on each patient's condition to determine the cause of their swallowing difficulties. From there, a personalized, integrated treatment plan is created, which may include therapies such as electrical stimulation, speech therapy, use of tongue pressure devices, and endoscopic evaluations. These treatments are combined with proper eating postures, dietary modifications in collaboration with nutritionists, and adjustments to food texture and consistency to make swallowing easier and reduce the risk of choking.
For younger individuals or those with early symptoms, performing swallowing and oral exercises can help maintain and improve swallowing function. The team conducts comprehensive assessments based on each patient's condition to determine the cause of their swallowing difficulties. From there, a personalized, integrated treatment plan is created, which may include therapies such as electrical stimulation, speech therapy, use of tongue pressure devices, and endoscopic evaluations. These treatments are combined with proper eating postures, dietary modifications in collaboration with nutritionists, and adjustments to food texture and consistency to make swallowing easier and reduce the risk of choking.
Additionally, aging is one of the primary causes of swallowing difficulties. The natural aging process is often accompanied by sarcopenia (muscle loss), which leads to the weakening of oral and tongue muscles or the deterioration of nervous system control over swallowing. As more societies enter the super-aged category, the prevalence of swallowing difficulties continues to climb. It is estimated that one in every ten elderly individuals will face such challenges.
Since aging is irreversible, does that mean a nasogastric tube is the only option for those who develop swallowing difficulties in old age? Dr. Jun-Jie Wu explains, "Aging cannot be reversed, but with proper medical care and swallowing training, we can delay or improve swallowing difficulties."
He provides an example: an 85-year-old patient with untreated swallowing issues might require a nasogastric tube immediately. However, with proper swallowing training, the need for a feeding tube could potentially be delayed until age 90. "Many elderly patients receiving palliative care or experiencing age-related decline may naturally reach the end of life during this period. This enables both patients and their families to avoid the difficult decision of whether to place a feeding tube, allowing the patient to maintain dignity until the very end," explains Dr. Wu.
Promoting Swallowing Awareness to Reduce Nasogastric Tube Placement
In addition to encouraging patients to recognize their own symptoms and seek timely care, Taipei City Hospital has incorporated its electronic medical system to proactively identify potential dysphagia cases. By analyzing data from both inpatients and outpatients, the system flags individuals at risk, enabling early intervention. The team also extends services to in-home palliative care and Taiwan's Long-Term Care 2.0 facilities.
Dr. Ya-Ling Li explains that some patients are unaware they have swallowing difficulties. They may misinterpret their poor appetite or trouble with solid foods as temporary effects of illness recovery and ask nurses to switch their meals to pureed or liquid diets. "At this stage, we can use data from the Nutrition Department to quickly identify patients with special dietary needs and notify their attending physicians for further evaluation," she says.
 To expand service capacity, the Taipei City Hospital's Multidisciplinary Swallowing Team secured funding from the Taipei City Department of Health, setting an annual goal of screening 1,000 potential dysphagia patients and visiting 1,000 diagnosed patients. Dr. Li explains, "Beyond helping more patients with swallowing difficulties, we also aim to raise public awareness about swallowing disorders and the importance of early intervention."
To expand service capacity, the Taipei City Hospital's Multidisciplinary Swallowing Team secured funding from the Taipei City Department of Health, setting an annual goal of screening 1,000 potential dysphagia patients and visiting 1,000 diagnosed patients. Dr. Li explains, "Beyond helping more patients with swallowing difficulties, we also aim to raise public awareness about swallowing disorders and the importance of early intervention."
Taiwan has an exceptionally high number of nasogastric tube users compared to other countries. Statistics show that approximately 450,000 to 500,000 people in Taiwan rely on nasogastric tubes, with usage in long-term care facilities reaching an astounding 94.05%—the highest globally. Dr. Ya-Ling Li points out that long-term nasogastric tube placement is extremely common in Taiwan, with some patients having used one for more than 10 years. "This is an exceptionally rare phenomenon in healthcare systems around the world," she remarks.
In reality, placing a nasogastric tube treats the symptoms but not the root cause. Research has increasingly shown that nasogastric tubes do not significantly reduce the risk of choking. "Saliva is still present in the mouth, and in fact, liquids are the substances most likely to cause choking," Dr. Li explains. She clarifies that nasogastric tubes are meant to be a temporary measure after a physician's evaluation—not a permanent solution. "Many people think that once a nasogastric tube is inserted, it can never be removed, but with integrated treatment and proper swallowing training, there is still a chance to resume eating by mouth or achieve what we call comfort feeding," she says.
Respecting Patient Wishes: The Concept of Comfort Feeding
"For terminal patients receiving palliative care, nutritional intake is not as crucial as it is for the general population. For them, being able to eat the foods they desire can be a deeply healing experience," says Dr. Li. By respecting patients' eating preferences and personal choices, the concept of comfort feeding promotes oral intake through small, frequent meals, allowing patients to experience the joy and dignity of eating without stress. Dr. Li further emphasizes, "The key to comfort feeding is the patient's own will—let them eat when they want to eat, and do not force them when they don't want to eat. It is essential to respect their wishes and how they feel physically."

Every patient has different expectations regarding treatment. Some, even after understanding the risks, are determined to have their feeding tube removed. Others do not insist on tube removal but simply wish to taste food again. The team engages in thorough discussions with patients and their families, clearly explaining the potential benefits of swallowing therapy, the risks of removing a feeding tube, and the significance of comfort feeding. Ultimately, treatment plans are tailored based on the patient's preferences.
Dr. Li shares the story of a terminally ill patient who had served as a diplomat and had been using a nasogastric tube for three years due to cancer. "His greatest wish was to once again enjoy a slice of cake and a cup of coffee, just like he used to." With the help of the team's treatment and training, he was first able to sip coffee through a dropper. In the final six months of his life, he successfully had his feeding tube removed and was finally able to savor the cake he had longed for.
Since its establishment, the Multidisciplinary Swallowing Team of Taipei City Hospital has actively promoted integrated care for swallowing disorders. To date, the team has successfully removed nasogastric tubes for over 400 patients, achieving an impressive 30% removal rate. This remarkable accomplishment earned the team the Symbol of National Quality (SNQ) award.
Dr. Li expresses gratitude that, after years of effort, public awareness and medical professionals' perspectives on swallowing disorders and feeding tubes have begun to shift. She hopes that through continued collaboration between the government and hospitals, swallowing awareness and comfort feeding can be further promoted. "We hope that when people reach the end of life, they won't need a feeding tube, but can instead enjoy their final meal in comfort and with dignity."
