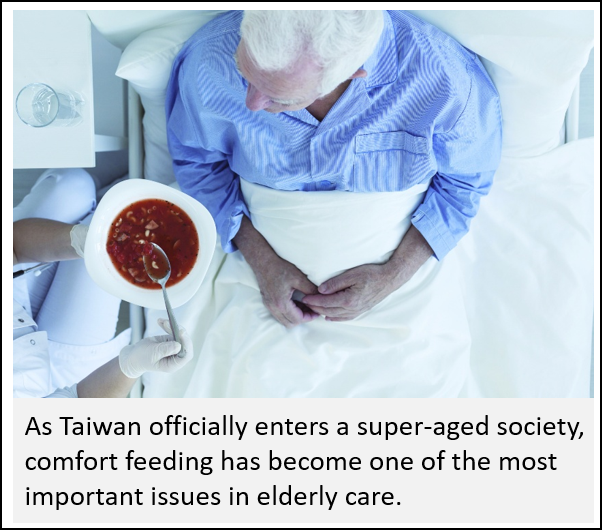
According to the latest population projection report, Taiwan’s elderly population will exceed 20% of the total population by 2025, officially entering a super-aged society. Many elderly individuals experience swallowing difficulties and malnutrition due to aging or illness, leaving families with the difficult decision of whether to insert a nasogastric tube. Ensuring that the elderly can eat comfortably and enjoy their meals until the very end of life has become one of the most important issues in elderly care today.
As Taiwan becomes a super-aged society, the National Health Insurance Administration officially included frail elderly individuals as eligible for palliative care benefits starting in June 2022. Dr. Yih-Chyang Weng, the director of the Radiation Oncology Department at Nantou Hospital and a long-time practitioner in the field of palliative care, has deep insights into this issue. He mentions that, when caring for frail elderly individuals, the challenges faced by palliative care teams are numerous, and one of the major concerns is feeding.
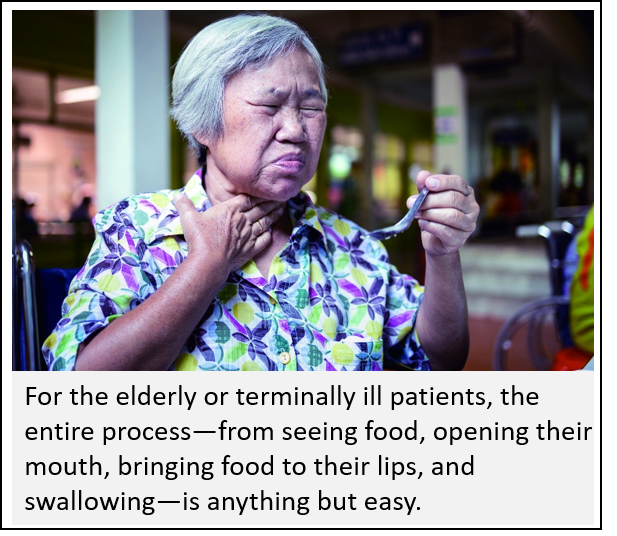
 "How can frail elderly individuals age naturally? Dietary care plays a crucial role," Dr. Weng explains. Citing various domestic and international studies, he points out that proper eating habits can slow brain degeneration, and maintaining a happy and engaged mind reduces cognitive decline—well-established concepts. In addition, the act of eating fulfills basic physiological needs, satisfies the senses of smell and taste, and brings joy to the soul. However, in reality, ensuring that frail elderly individuals, even those in the final stages of life, can enjoy eating is not easy. Among the greatest hurdles are difficulty swallowing and choking.
"How can frail elderly individuals age naturally? Dietary care plays a crucial role," Dr. Weng explains. Citing various domestic and international studies, he points out that proper eating habits can slow brain degeneration, and maintaining a happy and engaged mind reduces cognitive decline—well-established concepts. In addition, the act of eating fulfills basic physiological needs, satisfies the senses of smell and taste, and brings joy to the soul. However, in reality, ensuring that frail elderly individuals, even those in the final stages of life, can enjoy eating is not easy. Among the greatest hurdles are difficulty swallowing and choking.
Comfort Feeding: Professional Assistance as a Support
"Eating is a complex process," says Dr. Weng. For elderly or terminally ill patients, the act of eating—seeing the food, opening the mouth, placing the food into the mouth, and swallowing—is far from simple. Often, the first bite goes smoothly, and the second may also be swallowed without any problems. However, as eating continues, swallowing difficulties or choking may arise. These challenges are not necessarily related to the speed of feeding but rather to the patient’s progressive decline, resulting in a loss of the ability to continue eating. Balancing care for eating while providing end-of-life care has become one of the biggest challenges for palliative care teams.
Over the years, Dr. Weng has worked in clinical care and has gradually understood the challenges. He believes that to effectively reduce chewing and swallowing difficulties, regular oral hygiene care is essential to maintain a good eating state. Additionally, exercises like oral motor exercises and desensitization massages can effectively enhance oral muscle strength. Meanwhile, professional medical support is essential for adjusting and improving food textures to accommodate individual needs.
Dr. Weng explains that comfort feeding is an important aspect of achieving a dignified end-of-life experience, but families do not have to face this challenge alone: "Medical institutions, palliative care teams, and speech therapists can all provide professional assistance." Around 2010, the concept of comfort feeding was introduced from abroad as one of the important decisions toward a good death. It encourages shared decision-making between doctors and patients, further opening up collaboration between palliative care and swallowing therapy teams. This helps elderly individuals or patients with swallowing difficulties to retain the joy of eating during their final moments.
Currently, medical evaluations using imaging techniques and endoscopy are available to assess swallowing function. Taiwan’s National Health Insurance also covers food texture classification tests, allowing individuals to better understand the appropriate food consistency for their condition. Dr. Weng further explains that the International Dysphagia Diet Standardization Initiative (IDDSI) provides a global standard for food texture classification. This system categorizes food from liquids to solids into eight levels (ranging from 0 to 7). In addition to medical assessments, individuals can conduct simple texture tests at home using everyday utensils such as spoons, forks, or syringes to determine the most suitable food consistency.
The Happiness of Eating: Toward a Beautiful and Peaceful End
Enjoying food and eating until life’s final moments is a universal hope. It is also the professional focus of Hsiao-Ching Liu, a palliative care nursing educator at Dah-Der Hospice & Palliative Care Foundation. She has dedicated the past two years to studying and refining this aspect of care for patients.
Dame Cicely Saunders, the pioneer of modern hospice care, once said, "We will do everything we can not only to help you die peacefully, but also to live until you die." This quote made Liu reflect deeply, and after a long period of contemplation, she came to fully grasp its meaning: "It’s not about using every medical intervention to keep a patient alive until the very last moment, nor is it about removing a feeding tube without considering how to care for and support the patient’s nutrition afterward. Rather, it is about allowing them to live naturally and in harmony until the very end."
With 30 years of experience in nursing--24 years of which were specifically in hospice care--Liu reflects on her palliative care training and affirms that one of the most fundamental aspects of hospice education is comfort care, which includes oral hygiene and choking prevention. Over the past two decades, choking prevention methods have remained largely unchanged, mainly relying on food thickeners and proper positioning techniques to reduce the risk. However, these measures alone have proven insufficient in meeting the diverse needs in clinical settings.
 As Liu continues to deepen her understanding of comfort feeding, she realized that she still had a lot to learn. "I used to believe that using smaller spoons and cooking food until it became extremely soft was the best approach, but I later realized these were misconceptions. Even professional nursing knowledge needs to evolve. The use of food thickeners, as well as considerations of food texture, size, and portioning, all require careful evaluation," she explains.
As Liu continues to deepen her understanding of comfort feeding, she realized that she still had a lot to learn. "I used to believe that using smaller spoons and cooking food until it became extremely soft was the best approach, but I later realized these were misconceptions. Even professional nursing knowledge needs to evolve. The use of food thickeners, as well as considerations of food texture, size, and portioning, all require careful evaluation," she explains.
Once she changed her approach, her previously clouded perspective became clearer. Recently, she cared for a child with a rare disease who had to control his diet over a long period due to epilepsy medication. The child’s swallowing muscles had lost strength, and even drinking water caused choking. When Liu asked the child about his wishes, his answer made her heart tighten. "I don't want the feeding tube," he said, his eyes bright despite his condition." And I really want to eat fried chicken."
Determined to grant this wish, Liu rallied her team and enlisted the help of a nutritionist. After conducting tests to determine the appropriate food texture for the child, they carefully adjusted the consistency of the food. Days of effort finally led to the creation of a fried chicken drumstick that resembled the appearance, texture, and taste of the real thing.
Watching the child eat with delight--his eyes sparkling with joy despite the dark circles on his face-- Liu Xiao-Qing realized that maintaining the happiness of eating until the last moments of life is an essential part of a peaceful and meaningful end.
Enjoying Life: Eating as a Source of Vitality
Support from a medical team extends beyond doctors and nurses—it also includes speech therapists. "Many people are still unfamiliar with our role," says speech therapist Hsueh-Pei Wang with a smile. While speech therapists are often associated with helping patients regain communication abilities after conditions like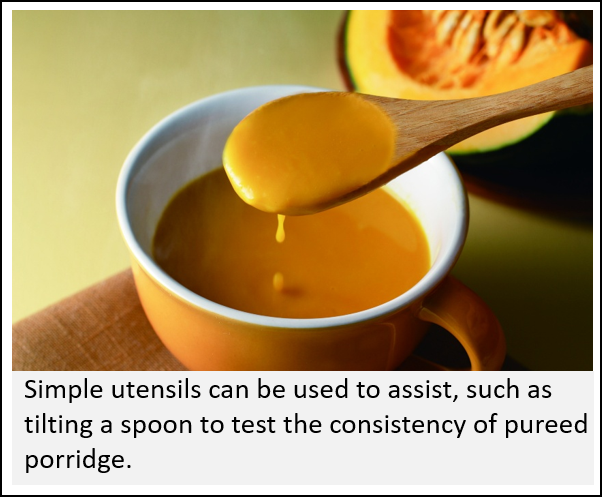 aphasia, their expertise goes far beyond that. They play an indispensable role in long-term care teams.
aphasia, their expertise goes far beyond that. They play an indispensable role in long-term care teams.
With the official inclusion of eating and swallowing care in the Long-Term Care 2.0 program, the public is gradually becoming aware of the role speech therapists play in swallowing treatment. They can assist elderly patients or individuals with swallowing difficulties by identifying the causes of choking and food refusal and finding precise solutions to these issues.
For the first ten years of her career, Wang worked in medical institutions, assisting patients with severe strokes and traumatic brain injuries in overcoming their difficulties and gradually transitioning them from nasogastric tubes to oral feeding. Over time, she realized that beyond those deemed more likely to recover, an increasing number of elderly people with dementia or frailty also needed care. Many of them or their families were even willing to pay out of pocket for therapy in hopes of delaying or avoiding the use of a feeding tube.
This realization led Wang to establish her own speech therapy practice, extending her services into home healthcare and elderly care facilities. She now dedicates her work to helping individuals with dementia, Parkinson’s disease, and age-related degeneration rediscover the joy of eating through the mouth.
This shift in perspective allowed Hsueh-Pei Wang to recognize the long-standing struggles faced by many patients and families. She once helped an elderly woman who had been reliant on a nasogastric tube for over a year regain the ability to eat by mouth. The woman's family had previously expressed frustration, saying that even though the food was blended into a purée, she would still choke and struggle to swallow.
After conducting a thorough assessment, Wang identified the issue: "Many assume that modifying food texture simply means blending it into a fine purée. However, swallowing is influenced by more than just food size—its softness, viscosity, and cohesiveness all play crucial roles. Speech therapists use physiological swallowing assessments to determine the most suitable texture for each patient."
Wang is deeply concerned, saying, "Sometimes, the issue isn't that an elderly person can't swallow—it's that we haven't found the right approach. Keeping a feeding tube in place indefinitely feels like such an unnecessary loss." Because food texture needs vary greatly among individuals, having a speech therapist assess safe dietary options can make a significant difference. For caregivers with limited time, there are also products available that can be used to create safe, tasty meals.
"By identifying the underlying causes and gradually training the muscles, people can maintain the joy of eating by mouth until the end of life. They can not only enjoy life but also continue to savor the experience of living!" Wang emphasizes.
"Eating is a source of happiness for patients, and for many families, it provides emotional comfort as well," Wang says. Over the years, she has witnessed too many elderly people—whether due to aging-related swallowing decline or disease-induced dysphagia—painfully spend their final days reliant on feeding tubes. "Once a patient stops eating by mouth, their swallowing function deteriorates further, eventually making even swallowing saliva a risk for aspiration pneumonia."
"Eating is the best swallowing exercise," Wang affirms. By identifying the case and finding the appropriate eating methods, people can continue to experience the pleasure of eating by mouth, allowing them to not just sustain life but to truly enjoy it.
The Rise of Care Foods: A New Opportunity for Comfort Feeding
Helping elderly individuals in the community regain the ability to eat by mouth is deeply fulfilling, but not without its challenges. As Hsueh-Pei Wang encountered more patients, she also faced the greatest challenge of her career.
"Elderly individuals tend to eat less as their illnesses progress. When swallowing becomes increasingly difficult, they are often placed on a nasogastric tube," Wang explains. As a speech therapist, she once had full confidence in her ability to help frail, elderly patients resume eating by mouth. However, she soon encountered an overwhelming obstacle: "Stroke patients may suffer physical impairments due to their condition, but their situation does not continuously worsen. Frailty, on the other hand, is irreversible. Patients often deteriorate due to multiple health issues, requiring constant adjustments to swallowing interventions."
Faced with this challenge, Wang refused to give up. The more she studied comfort feeding solutions, the more her perspective expanded.
"I kept asking myself—do patients truly lose the ability to eat, or have we simply not tried every possible method?" Through the promotion of the International Dysphagia Diet Standardization Initiative (IDDSI), Wang discovered just how crucial food texture is. Factors like cohesiveness, viscosity, size, and softness are meticulously classified into different categories. Around this time, she came across research on Japan's emerging care food approach—a technique that uses special Japanese enzymes to transform food into a molded, gel-like consistency.
Inspired by this approach, Wang applied the method to an elderly woman who had been reliant on a nasogastric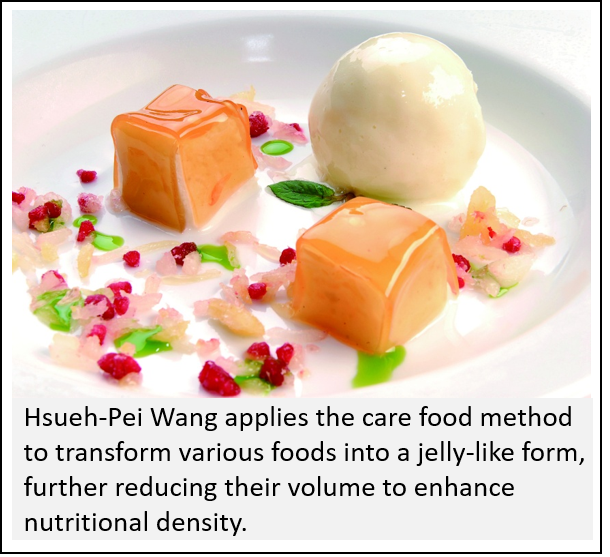 tube for over a year. After conducting a swallowing assessment, she guided the family in preparing molded gel-like food, adjusting its smoothness and cohesiveness to match the patient's physiological condition. A nutritionist was also consulted to ensure proper nutritional density. After two months of effort, the elderly woman successfully had her feeding tube removed. This approach not only preserved the original flavors of the food while making it safe for consumption but also brought immense joy to both the patient and her family. The success of this case deeply encouraged Wang.
tube for over a year. After conducting a swallowing assessment, she guided the family in preparing molded gel-like food, adjusting its smoothness and cohesiveness to match the patient's physiological condition. A nutritionist was also consulted to ensure proper nutritional density. After two months of effort, the elderly woman successfully had her feeding tube removed. This approach not only preserved the original flavors of the food while making it safe for consumption but also brought immense joy to both the patient and her family. The success of this case deeply encouraged Wang.
Since then, she has helped many more elderly individuals regain the ability to eat by mouth. One of her most rewarding moments came recently when a patient with severe Parkinson's disease, who had been unable to eat solid food for years, was finally able to enjoy his favorite Hong Ye cake again on Father's Day—a tradition he had dearly missed.
Recreating Authentic Flavors
After making significant progress in food texture modification, Hsueh-Pei Wang made another key observation: when elderly individuals were presented with foods they loved, their willingness to eat increased significantly. This realization led her to experiment with transforming familiar dishes—softening pork knuckles or turning them into gel-like forms, and even reducing portion sizes while increasing nutritional density. This way, even those with limited appetites could still receive adequate nutrition. Her bold approach proved to be highly effective.
Smiling, she remarks, "We've found foods that can serve as meal replacements while still providing enough nutrition, calories, and hydration—and they're foods the elderly actually enjoy eating. Isn't that perfect?" Wang dedicated herself to helping seniors in the community rediscover the joy of eating, while her colleague, Hsiao-Ching Liu, remained committed to palliative care patients in medical institutions. Liu faced even greater challenges—after all, in hospice care, patients' lifespans and physiological conditions were far more fragile and urgent than those of the frail elderly. Sometimes, before a swallowing assessment could even be completed, the patient had already passed away, making every moment a race against time.
One of Liu's patients was a 108-year-old woman with severe frailty. Due to multiple episodes of aspiration pneumonia, the care facility had placed her on a nasogastric tube to ensure adequate nutrition. To prevent her from pulling out the tube, they also fitted her with protective mittens.
 "Those mittens—the ones with hard plates or metal inserts inside—are incredibly uncomfortable," Liu says. Fortunately, the woman's family did not want her to spend her final days in such an undignified manner. They decided to remove the feeding tube, take off the mittens, and bring her home for proper care. However, despite their patience and careful planning, feeding her remained a major challenge.
"Those mittens—the ones with hard plates or metal inserts inside—are incredibly uncomfortable," Liu says. Fortunately, the woman's family did not want her to spend her final days in such an undignified manner. They decided to remove the feeding tube, take off the mittens, and bring her home for proper care. However, despite their patience and careful planning, feeding her remained a major challenge.
"When she arrived at the hospice ward, we noticed that she still had the desire to eat. However, she choked easily and lacked the strength to cough." Recognizing this, Liu immediately activated the comfort feeding care model, collaborating with specialists and urgently requesting samples from a Taiwanese care food manufacturer. "On the day before she passed away, she ate two high-nutrition puddings and kept opening her mouth for more."
The scene deeply moved everyone present, including the medical team and the elderly woman's loved ones. After her passing, her granddaughter held Liu's hand and said, "Thank you for allowing Grandma to eat what she wanted in her final moments."
That one sentence struck Liu deeply, reinforcing her determination to continue advocating for comfort feeding. "She was able to enjoy food the day before she passed away. But if we had introduced these options earlier, the happiness she experienced could have lasted longer."
Determined to make a change, Liu partnered with Wang and collaborated with the Taiwan Society of Home Health Care to expand awareness. In December 2022, they held their first online seminar on comfort feeding. "Due to bandwidth limitations, we could only accept 100 participants, and it filled up instantly. Afterward, so many people complained that they couldn't get in," Liu recalls with a smile. Despite the unexpected demand, both women felt overjoyed—it was proof that the need for comfort feeding was far greater than they had imagined.
Wang also noted that as societies continue to age, more people will experience swallowing and chewing difficulties. "The concept of comfort feeding shouldn't be limited to speech therapists or rehabilitation doctors—it needs to reach the entire healthcare team and the general public."
She acknowledged that comfort feeding is still a relatively new idea, but its rapid adoption has been surprising. "In the past, families would ask if we could help their loved ones eat until the very end. But now, during consultations, they're the ones saying, 'I want my parents to experience comfort feeding.' That's incredibly moving."
Looking ahead, both Liu and Wang recognize that the journey is long, but they remain confident. Beyond raising awareness, they are considering launching cooking courses to turn the concept of comfort feeding into a practical reality—helping caregivers create meaningful, harmonious moments for their loved ones through the joy of eating.